Neurofeedback therapy targets the brain's reward system by utilizing real-time monitoring of brainwave activity to train individuals to self-regulate their brain function. By focusing on specific brainwave patterns associated with the reward system, such as beta and theta waves, neurofeedback aims to modulate the neural pathways involved in substance abuse. Through operant conditioning, individuals learn to regulate their brain activity, leading to improved self-control and reduced cravings for substances.
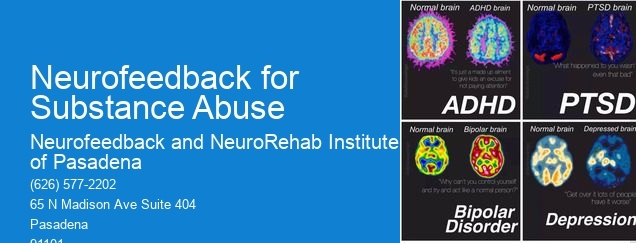
The specific neurophysiological mechanisms through which neurofeedback helps individuals with substance abuse disorders involve the modulation of neural networks associated with reward processing, impulse control, and emotional regulation. Neurofeedback aims to enhance the functioning of the prefrontal cortex, which plays a crucial role in decision-making and impulse control, while also targeting the limbic system, involved in emotional responses and reward processing. By promoting self-regulation of these brain regions, neurofeedback can help individuals better manage the underlying neurobiological factors contributing to substance abuse.
Respiration RateNeurofeedback can be tailored to address the specific neurotransmitter imbalances associated with different types of substance abuse. Alpha Waves For example, in cases of opioid addiction, neurofeedback may target the brain's endorphin system, while for alcohol dependence, it may focus on GABAergic and glutamatergic pathways. By customizing neurofeedback protocols to address individual neurotransmitter imbalances, this therapy can potentially offer targeted support for various substance abuse disorders.
Neurofeedback therapy addresses the underlying emotional and psychological factors contributing to substance abuse by promoting self-regulation of brain activity in regions associated with emotional processing and regulation. By training individuals to modulate their brainwave patterns, neurofeedback can help reduce anxiety, depression, and impulsivity, which are often intertwined with substance abuse. This self-regulation can lead to improved emotional resilience and coping strategies, supporting long-term recovery.
Delta WavesSpecific brainwave patterns targeted and modified through neurofeedback to support recovery from substance abuse include alpha, beta, theta, and sensorimotor rhythm (SMR) frequencies. These brainwave patterns are associated with attention, relaxation, impulse control, and emotional regulation. Brain Mapping By training individuals to modulate these specific brainwave patterns, neurofeedback aims to enhance cognitive function, emotional stability, and self-control, which are essential for overcoming substance abuse.

There are specific protocols and guidelines for using neurofeedback as part of a comprehensive treatment plan for substance abuse. These protocols involve initial qEEG (quantitative electroencephalography) assessments to identify individualized neurofeedback targets, followed by a series of neurofeedback sessions tailored to the individual's brainwave patterns. The treatment plan may also include regular progress evaluations and adjustments to the neurofeedback protocols based on the individual's response.
Neurofeedback therapy can integrate with other evidence-based treatments for substance abuse, such as cognitive-behavioral therapy (CBT) or medication-assisted treatment (MAT). When combined with CBT, neurofeedback can address both the cognitive and neurophysiological aspects of substance abuse, offering a comprehensive approach to recovery. Additionally, neurofeedback can complement MAT by targeting the underlying neural mechanisms contributing to substance dependence, potentially enhancing the overall effectiveness of the treatment plan.
EEG Biofeedback Software
Neurofeedback has shown promising results in addiction treatment, with studies indicating that it can be effective in reducing cravings, improving emotional regulation, and enhancing overall well-being. Research has suggested that neurofeedback may help individuals with addiction by targeting specific brain regions associated with reward processing, impulse control, and decision-making. By training the brain to self-regulate and function more efficiently, neurofeedback has the potential to support long-term recovery from addiction. While individual success rates may vary, many individuals have reported positive outcomes from incorporating neurofeedback into their addiction treatment plans. Further research and clinical trials are ongoing to better understand the specific mechanisms and efficacy of neurofeedback in addiction treatment.
Neurofeedback therapy has shown promise in benefiting both patients and caregivers in Alzheimer's disease cases. By utilizing neurofeedback techniques, individuals with Alzheimer's may experience improvements in cognitive function, memory retention, and overall quality of life. This can lead to a reduction in caregiver burden and an enhanced sense of well-being for both the patient and their caregivers. The use of neurofeedback may also contribute to a more positive caregiving experience by potentially reducing stress, anxiety, and depression among caregivers. Additionally, the potential for improved communication and interaction between the patient and caregiver may further enhance the overall care dynamic. Overall, neurofeedback therapy holds potential benefits for both patients and caregivers in the context of Alzheimer's disease.
Yes, there are neurofeedback programs specifically designed to help manage bipolar disorder in children. Neurofeedback, also known as EEG biofeedback, is a non-invasive treatment that aims to regulate brain activity and improve self-regulation. These programs often involve monitoring brainwave patterns and providing feedback to help children learn to self-regulate their emotions and behavior. Neurofeedback for bipolar disorder in children may focus on enhancing mood stability, reducing impulsivity, and improving attention and focus. It can be a valuable adjunct to traditional treatments such as medication and therapy, offering a more holistic approach to managing the symptoms of bipolar disorder in children.
The recommended duration of neurofeedback treatment for PTSD can vary depending on the individual's specific needs and response to the therapy. Typically, a course of neurofeedback treatment for PTSD may involve regular sessions over a period of several months to a year. The frequency and duration of sessions may be tailored to the severity of the PTSD symptoms, the individual's progress, and their overall treatment plan. It's important for the neurofeedback therapist to continually assess and adjust the treatment protocol based on the client's ongoing response and needs. Additionally, integrating complementary therapies and support services alongside neurofeedback may further enhance the overall treatment outcomes for individuals with PTSD.
Neurofeedback has shown promise in supporting individuals with Alzheimer's disease in maintaining cognitive function. By utilizing advanced brainwave monitoring and training techniques, neurofeedback can target specific neural pathways associated with memory, attention, and executive function, which are often affected by Alzheimer's disease. This non-invasive approach aims to modulate brain activity, enhance neural plasticity, and promote neurogenesis, potentially mitigating cognitive decline. Furthermore, neurofeedback interventions can be tailored to address individual cognitive deficits, offering personalized and targeted support for those with Alzheimer's disease. Research suggests that neurofeedback may contribute to improved cognitive performance, memory retention, and overall quality of life for individuals living with Alzheimer's disease. While further studies are needed to fully understand the long-term effects, neurofeedback presents a promising avenue for enhancing cognitive function in this population.
Neurofeedback therapy has shown promise as an effective approach for addressing postpartum depression. Research suggests that this non-invasive treatment, which involves training the brain to regulate its own activity, may help alleviate symptoms such as mood swings, anxiety, and fatigue commonly associated with postpartum depression. By targeting specific brainwave patterns and promoting self-regulation, neurofeedback therapy aims to restore emotional balance and improve overall well-being. While further studies are needed to fully establish its efficacy, preliminary findings indicate that neurofeedback therapy could be a valuable addition to the range of treatment options available for postpartum depression.